A devastating humanitarian crisis is unfolding in Gaza’s maternity wards, where newborn mortality rates have skyrocketed by 75% according to alarming new data from the United Nations Children’s Fund (UNICEF). The agency’s comprehensive assessment reveals that between July and September, neonatal facilities recorded approximately 47 infant deaths monthly—a dramatic increase from the pre-conflict monthly average of 27 documented throughout 2022.
The nutritional crisis affecting pregnant women has created a cascading health emergency. UNICEF’s Tuesday briefing disclosed that 38% of screened pregnant women received diagnoses of acute malnutrition, with at least 8,300 expectant and breastfeeding women requiring emergency nutritional treatment in October alone. This maternal health catastrophe has directly impacted newborn outcomes, with the number of underweight infants (below 2.5 kilograms) nearly doubling from 250 monthly cases in 2022 to approximately 460 currently.
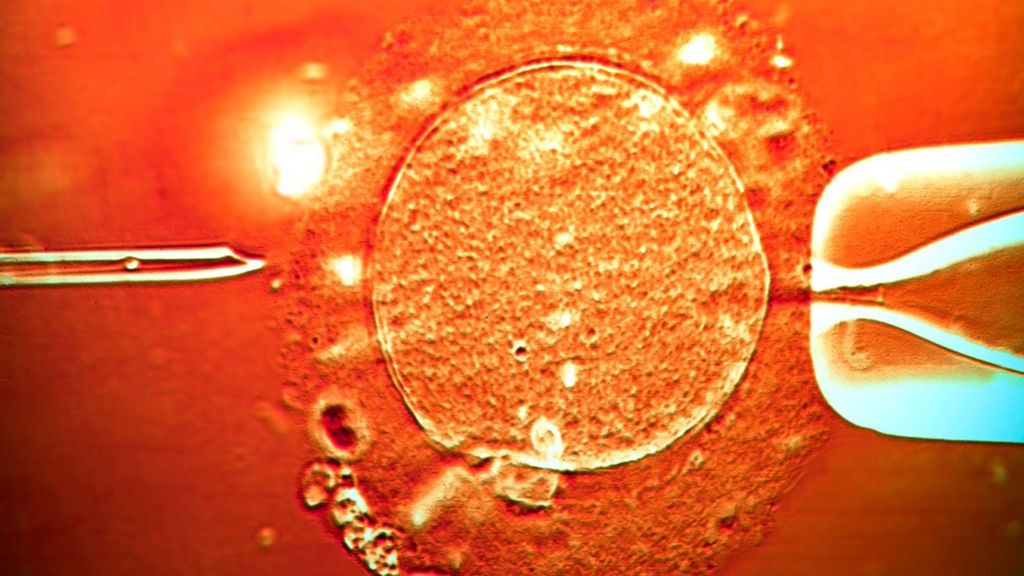
Medical professionals emphasize the grave implications of low birth weight, as these vulnerable infants face mortality risks 20 times higher than those born at healthy weights. UNICEF communications manager Tess Ingram provided firsthand testimony from Gaza’s hospitals, describing newborns weighing less than one kilogram struggling for survival. ‘The unmistakable pattern of malnourished mothers giving birth to premature or underweight infants represents a preventable tragedy,’ Ingram stated, noting that this suffering ‘could have been prevented if international humanitarian law had been respected.’
The healthcare collapse exacerbates the crisis, with Israeli authorities repeatedly blocking medical delegations and restricting aid shipments. Despite ceasefire agreements, only 14,534 aid trucks have entered Gaza since October—less than half of the 37,200 trucks required for basic humanitarian relief. This systematic obstruction has contributed to over 450 documented deaths from starvation and dehydration, including more than 154 children.
UNICEF officials report that 9,300 children across Gaza were identified as acutely malnourished in October, creating a generational health crisis that will likely result in lifelong complications for survivors. The agency continues urgent appeals for unimpeded humanitarian access, particularly for nutritional support targeting pregnant women and essential medical equipment for neonatal intensive care units.