A resident of New York’s Long Island suburbs has tested positive for chikungunya, a mosquito-borne virus typically prevalent in South America. This marks the first locally acquired case in the U.S. mainland since 2015, raising concerns among health officials. The patient, who began experiencing symptoms in August, had recently traveled within the country but not internationally. While the exact location of the mosquito bite remains unclear, the virus has not been detected in local mosquito populations, and it is not transmitted directly between humans. Chikungunya, first identified in Tanzania in 1952, derives its name from the Makonde language, meaning “that which bends up,” due to the severe joint pain it can cause. Symptoms include fever, muscle pain, nausea, fatigue, and rash, with rare cases leading to prolonged joint pain or organ damage. Although severe cases and fatalities are uncommon, they primarily affect infants and the elderly with underlying health conditions. There is no specific treatment for chikungunya, but symptom management includes fever reducers and pain relievers. Two vaccines are approved in regions like Europe and Brazil but are not widely available in highly affected areas. Globally, chikungunya outbreaks have surged since 2000, with over 317,000 cases and 135 deaths reported in 2024 alone, primarily in Brazil, Bolivia, Argentina, and Peru. Health officials attribute the rise in mosquito-borne diseases like chikungunya, dengue, and Zika to climate change and urban expansion. In New York, the Aedes albopictus mosquito, known to transmit the virus, is present in downstate areas, though current cooler temperatures reduce transmission risks. The CDC has recorded 199 travel-related cases in 2024, highlighting the need for vigilance in mosquito prevention measures.
分类: health
-

New Africa CDC platform boosts regional health manufacturing
The Africa Centres for Disease Control and Prevention (Africa CDC) has introduced the African Manufacturing Market Intelligence & Network Analysis (AMMINA) platform, a groundbreaking initiative designed to enhance health manufacturing, innovation, and self-reliance across the continent. Launched during the African Healthcare Manufacturing Trade Exhibition and Conference in Accra, Ghana, the platform aims to bolster health sovereignty and reduce Africa’s dependency on imported medical supplies. Jean Kaseya, Director-General of Africa CDC, emphasized that AMMINA will provide comprehensive data on manufacturers, production capacities, product portfolios, and market trends, enabling informed decision-making and fostering industrial growth. Initially, the platform maps data from over 700 manufacturers and 2,500 health products across 18 African Union (AU) Member States, with plans to expand coverage to all 55 Member States. AMMINA is expected to stimulate intra-African trade, attract sustainable investments, and drive innovation in local production of vaccines, medicines, and diagnostics. Africa CDC, in collaboration with AU institutions and partners, envisions AMMINA as a pivotal tool to unlock Africa’s manufacturing potential and secure the continent’s health future. This initiative comes as African nations strive to build a resilient health ecosystem, particularly in the wake of the COVID-19 pandemic, which highlighted vulnerabilities in global supply chains.
-

South Africa’s health minister hails new HIV prevention jab but warns of limited supply
South Africa’s Health Minister, Aaron Motsoaledi, has hailed the introduction of lenacapavir, the world’s first twice-yearly HIV prevention injection, as a groundbreaking development in the fight against the disease. However, he cautioned that the initial supply, funded by a $29.2 million Global Fund grant and an additional $5 million from the Networking HIV and AIDS Community of Southern Africa (NACOSA), will be limited to nearly half a million people in the country with the highest HIV prevalence rate. The rollout is scheduled to begin in April 2026, targeting 23 high-incidence districts across six provinces and 360 high-performing public clinics. Motsoaledi emphasized that prioritizing vulnerable populations in high-burden areas would maximize the impact in preventing new infections. The announcement follows the U.S. government’s recent pledge to purchase 2 million doses of the drug for low-income countries. Despite the optimism, Motsoaledi warned against complacency, citing the severe impact of abrupt funding cuts from USAID and other U.S. sources in early 2025 on HIV/AIDS and tuberculosis programs. While Gilead Sciences has reduced the annual cost of lenacapavir to $40 per person, South Africa aims to fund the program independently, with long-term sustainability dependent on integrating the drug into local systems. The World Health Organization has endorsed lenacapavir as an additional prevention option, and Gilead is expediting its registration in 18 high-incidence countries, including South Africa, until generic versions become available in 2027. However, the exclusion of South African manufacturers from Gilead’s voluntary licensing agreements has sparked criticism, with civil society leaders accusing the company of neglecting principles of fairness and inclusivity. Despite these challenges, UNAIDS has welcomed the investment, highlighting the potential of long-acting injectable medicines to reduce barriers to HIV prevention and expand choices for at-risk populations.
-

Foul skies, fading light: How air pollution is stealing India’s sunshine
India is grappling with a severe air pollution crisis, now ranking among the world’s top 10 most polluted countries. A recent study by six Indian scientists reveals that sunshine hours—the duration of direct sunlight reaching the Earth’s surface—have steadily declined across most of India over the past three decades. Published in *Scientific Reports*, the study analyzed data from 20 weather stations between 1988 and 2018, showing a nationwide reduction in sunshine hours, with only the northeast region experiencing mild seasonal relief. The steepest declines were observed in northern inland cities like Amritsar and Kolkata, as well as along the Himalayan belt and the west coast, particularly Mumbai. Seasonal patterns revealed significant increases in sunshine from October to May, followed by sharp drops from June to July in six of India’s nine regions. This decline is linked to India’s long-standing air pollution crisis, driven by rapid urbanization, industrial growth, and biomass burning, which have increased aerosol emissions and cloud formation. Aerosols have reduced sunlight reaching the ground by 13%, while clouds accounted for an additional 31-44% drop in surface solar radiation between 1993 and 2022. The study highlights concerns for agriculture, daily life, and India’s solar energy ambitions, with air pollution reducing solar panel output by 12-41% and costing an estimated $245-835 million in lost power generation. Cleaner air could boost India’s annual solar energy production by 6-28 terawatt hours, enough to power millions of homes. However, the impact of pollution extends beyond energy, causing significant crop yield losses in rice and wheat. While global trends show a rebound in sunlight due to cleaner air, heavily polluted countries like India are missing out, risking their renewable energy goals and overall development.
-
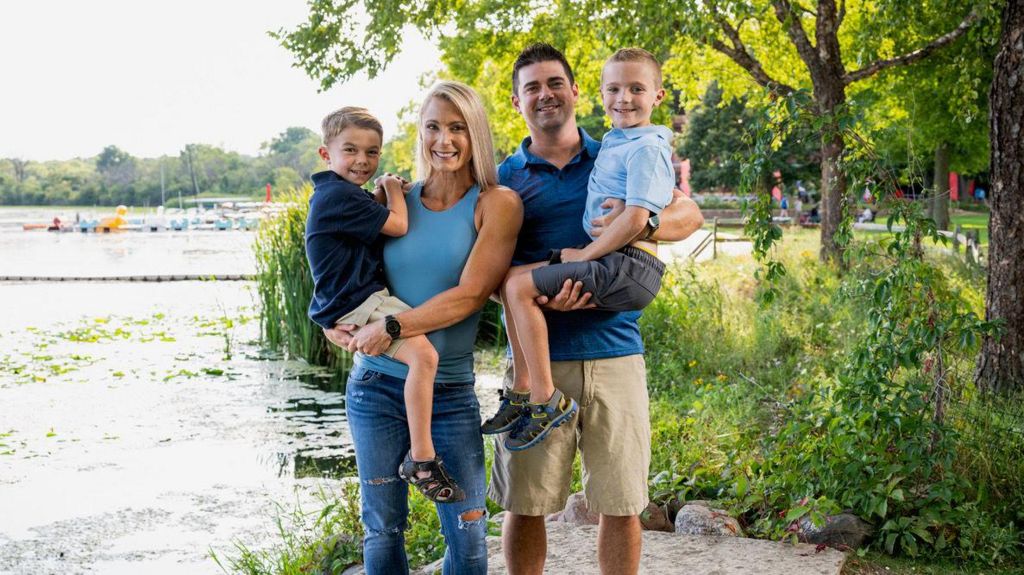
‘A lifeline’ – Americans fear spike in healthcare costs, making Republicans nervy
Shana Verstegen, a fitness trainer from Wisconsin, has been grappling with anxiety over the potential loss of her family’s health insurance subsidies under the Affordable Care Act (ACA). Alongside her husband, who also works as a fitness trainer, Verstegen relies on ACA premium tax credits to afford their health insurance, saving them approximately $800 monthly. However, these subsidies are set to expire at the end of the year, placing them at the center of a heated political battle amid the ongoing U.S. government shutdown. Democrats have refused to support any spending deal unless Republicans agree to renew the subsidies, leaving millions of Americans like Verstegen in limbo. Health policy experts warn that the expiration of these credits could lead to a significant spike in insurance premiums, making coverage unaffordable for many. Leighton Ku, a professor at George Washington University, estimates that premiums could double for the roughly 24 million Americans who rely on the ACA Marketplace, with up to seven million potentially dropping their coverage altogether. The impact would be particularly severe in Republican-leaning states that have not expanded Medicaid eligibility, disproportionately affecting working-class families who do not qualify for government assistance. Elizabeth Fowler, a scholar at Johns Hopkins, warns of a ‘death spiral’ in the insurance market, where rising premiums drive healthier individuals out, further increasing costs for those who remain. While some Republican leaders, including Senator Lisa Murkowski, have proposed extending the subsidies, the broader party remains divided. The looming November 1 open enrollment deadline adds urgency to the situation, as insurers have already adjusted rates in anticipation of the subsidies’ expiration. For families like Verstegen’s, the financial consequences could be devastating, forcing them to make significant sacrifices to maintain coverage. The political fallout from this issue could also be substantial, with experts suggesting that rising insurance costs in Republican districts may become a liability for the party in future elections.
-
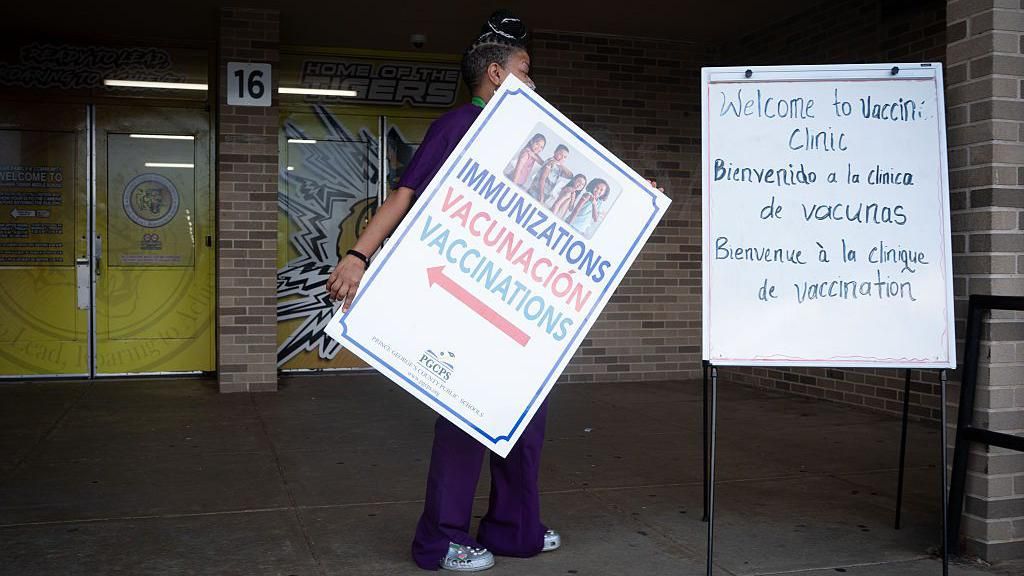
More than 150 schoolchildren quarantined as US measles cases hit 33-year high
In a concerning development, more than 150 unvaccinated schoolchildren in South Carolina have been placed under a 21-day quarantine following exposure to measles, according to state health officials. The affected students, who attend Global Academy of South Carolina and Fairforest Elementary in Spartanburg County, were forced to miss school due to their lack of immunizations during the period of potential disease transmission. This incident marks the latest in a series of measles outbreaks across the United States, with South Carolina reporting its eighth confirmed case in two weeks in Greenville County. The state’s Department of Public Health emphasized the urgency of measles vaccinations, citing active community transmission in the Upstate region. The MMR vaccine, which is 97% effective against measles, mumps, and rubella, remains the most reliable defense against the disease, which can lead to severe complications such as pneumonia, brain swelling, and even death. Meanwhile, measles cases are also surging in Utah and Arizona, with 55 and 63 cases reported, respectively. Nationwide, the U.S. has confirmed 1,563 cases this year—the highest in over three decades, according to the Centers for Disease Control and Prevention (CDC). This alarming trend follows earlier outbreaks in Texas and New Mexico, where hundreds were infected, and three fatalities occurred. The majority of cases involve unvaccinated individuals, highlighting the critical role of immunization in preventing the spread of this highly contagious disease. Globally, measles outbreaks have been reported in 100 countries over the past five years, with Canada experiencing a particularly severe surge, logging 5,024 cases—more than triple the U.S. total despite its smaller population. The situation has raised questions about the effectiveness of containment efforts and the impact of vaccine skepticism.
-

Shamans openly using psychedelic drugs for treatment in South Africa
In the lush outskirts of Cape Town, a clandestine yet burgeoning industry thrives despite stringent legal prohibitions. Psychedelic substances such as psilocybin and MDMA, though illegal in South Africa, are being openly utilized by self-proclaimed healers and shamans for therapeutic purposes. These practitioners, operating in a legal grey area, offer treatments that they claim can address a spectrum of mental health issues, from depression to PTSD.
-
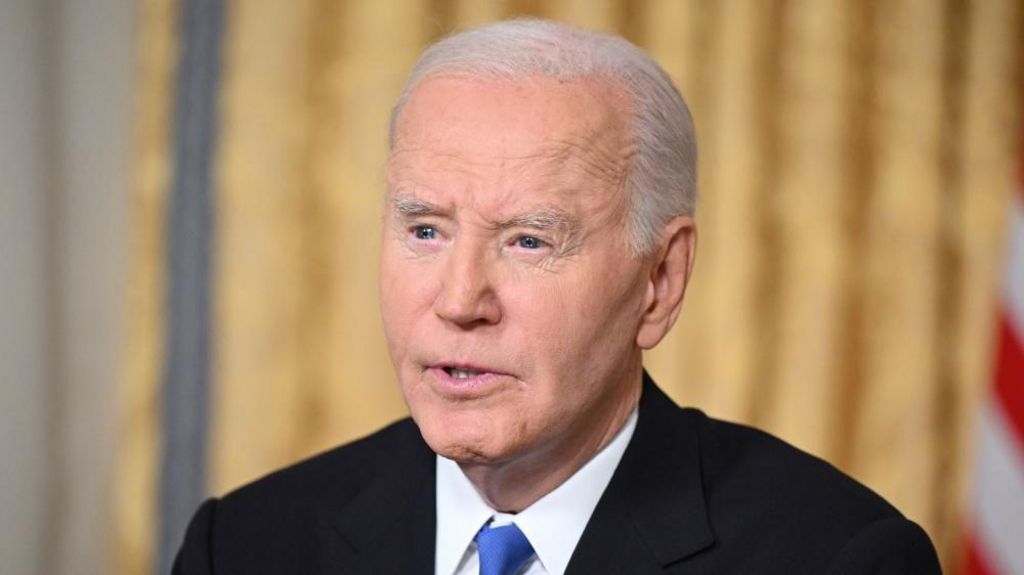
Biden receiving radiation therapy for prostate cancer
Former U.S. President Joe Biden has commenced radiation therapy as part of his ongoing treatment for prostate cancer, according to a statement from his spokesperson. The 82-year-old is also receiving hormone therapy, though specific details regarding this treatment remain undisclosed. A source familiar with the matter revealed to NBC News that the radiation therapy is expected to last five weeks, marking a significant phase in his medical care. Biden was diagnosed in May with an aggressive form of prostate cancer, which had metastasized to his bones. The diagnosis followed urinary symptoms that prompted medical examinations, leading to the discovery of a small nodule on his prostate. At the time, Biden’s office described the cancer as having a Gleason score of 9 (Grade Group 5), indicating a high-grade, fast-spreading form of the disease. However, the cancer is hormone-sensitive, which allows for effective management. Biden, who left office in January as the oldest serving U.S. president in history, faced persistent health concerns during his first term, ultimately leading him to withdraw from the 2024 re-election campaign. His former vice president, Kamala Harris, subsequently ran as the Democratic presidential candidate but lost to current President Donald Trump.
-

WHO flags regulation gaps after India child deaths from cough syrups
The World Health Organization (WHO) has expressed profound concern regarding lapses in India’s drug safety regulations following the tragic deaths of at least 20 children linked to contaminated cough syrups. The fatalities, reported in Madhya Pradesh and Rajasthan over the past month, have been traced to three specific syrups—Coldrif, Respifresh, and ReLife—found to contain diethylene glycol (DEG), a toxic chemical commonly used in industrial solvents. The Indian government has responded by arresting the owner of Sresan Pharmaceuticals, the manufacturer of Coldrif, halting production, and initiating a comprehensive investigation. The WHO has also warned that these tainted medicines could potentially reach other countries through unregulated distribution channels. In Tamil Nadu, health authorities have permanently revoked the manufacturing license of Sresan Pharmaceuticals after an inspection revealed 364 violations, including unhygienic storage conditions, substandard water quality, and lack of quality assurance protocols. The incident has sparked national outrage and raised concerns among parents, as oral syrups are commonly administered to children in India. This is not the first time Indian-made cough syrups have come under scrutiny; similar cases in The Gambia and Uzbekistan in 2023 resulted in the deaths of 88 children. The recurring issue highlights systemic failures in India’s pharmaceutical regulatory framework and underscores the urgent need for stricter oversight and accountability.
-

Senegal records 17 deaths in rare major outbreak of Rift Valley Fever
Senegal is grappling with a severe outbreak of Rift Valley Fever (RVF), a viral disease that has claimed 17 lives and infected 119 individuals, according to health officials. The outbreak, primarily concentrated in the northern livestock-producing region, marks the country’s most significant RVF crisis since the late 1980s. Dr. Boly Diop, head of RVF surveillance at Senegal’s health ministry, expressed concerns about the potential for further spread, emphasizing the unprecedented scale of the current outbreak. RVF, which primarily affects animals, can be transmitted to humans through mosquito bites or direct contact with infected livestock. While most human cases are mild or asymptomatic, severe infections can lead to eye damage, brain swelling, or fatal hemorrhagic fever, as reported by the World Health Organization (WHO). High-risk groups include herders, farmers, and slaughterhouse workers, who are often exposed during animal handling. The current outbreak was officially declared on September 21, with experts linking its resurgence to climate change, which creates favorable conditions for disease-carrying vectors. Dr. Merawi Aragaw Tegegne, an epidemiologist with the Africa Center for Disease Control and Prevention, highlighted the role of extreme weather patterns, such as torrential rains and floods, in facilitating RVF transmission. Preventive measures, including livestock vaccination and mosquito control, are crucial to curbing the disease’s spread. Historically, RVF has caused significant fatalities in Africa, with outbreaks in Kenya and Somalia in 1998 claiming over 470 lives. In 2000, the virus expanded beyond Africa, reaching Saudi Arabia and Yemen and raising global concerns about its potential spread to other continents.
