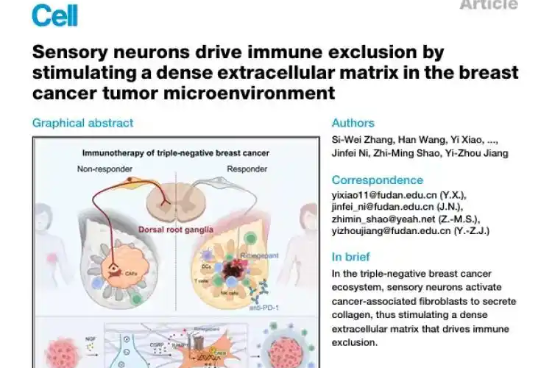
A groundbreaking study led by Chinese scientists has identified a previously unknown mechanism behind treatment resistance in one of the most aggressive forms of breast cancer. Published in the prestigious journal Cell, the research reveals how sensory nerves within tumors actively block immunotherapy effectiveness in triple-negative breast cancer (TNBC) patients.
The research team from Fudan University Shanghai Cancer Center and the Institute for Translational Brain Research made a paradigm-shifting discovery by examining the tumor microenvironment rather than focusing exclusively on cancer cells themselves. Their analysis of 360 clinical samples demonstrated that tumors with significant sensory nerve infiltration consistently showed the poorest patient outcomes.
According to lead researcher Dr. Shao Zhimin, director of general surgery at the center, these sensory nerves—typically responsible for transmitting touch and pain sensations—effectively prevent immune cells from penetrating the core regions of tumors. The study details how cancer cells communicate with these nerves, triggering nearby cells to produce dense collagen barriers that physically block immunotherapies from reaching their targets.
The research offers immediate clinical implications through the experimental use of rimegepant, an already-approved migraine medication. In animal models, this drug successfully disrupted nerve signaling pathways, simultaneously slowing cancer progression and restoring immunotherapy effectiveness. Because rimegepant has established safety profiles and regulatory approval, researchers believe these findings could rapidly transition to human clinical trials.
Dr. Jiang Yizhou, another lead expert on the project, emphasized that the collagen barrier acts as a physical wall protecting cancer cells from immune attack. The study fundamentally changes how scientists approach cancer treatment by demonstrating the critical integration between nervous and immune systems in tumor development and treatment resistance.
This discovery represents a significant advancement in oncology, particularly for TNBC patients who account for approximately 20% of breast cancer cases and face limited treatment options due to the cancer’s aggressive nature and tendency to metastasize rapidly.